Abstract: When the severe acute respiratory syndrome (SARS) epidemic hit Hong Kong 17 years ago, the author led the effort to rapidly transform the large acute tertiary Princess Margaret Hospital into a SARS hospital. Today, COVID-19 has overwhelmed healthcare systems worldwide. This serious event causes us to reflect on how to prevent similar failures in future pandemics. Here, the author shares her 2003 SARS experience in designing an infectious disease hospital to enable isolation and prevent viral transmission, also her recent experience in building community quarantine centers to contain and isolate close contacts of COVID-19 patients to mitigate community outbreak. Effective infection control measures are key to protecting valuable healthcare resources, but these measures must be well-designed and readily available when required. Future hospitals should be flexibly designed to be sustainable under normal circumstances, yet agile enough to transform into infectious disease isolation facilities during a pandemic.
Keywords: SARS, COVID-19, infection control, Infectious Disease Center, Community Quarantine Centers.
1. Introduction
The 1918 Spanish flu outbreak swept across the world near the end of World War I with a devastating global impact. Between February 1918 and April 1920, 500 million people (approximately one-third of the world’s population at the time) became infected in four successive waves, and between seventeen and fifty million people died, making it one of the deadliest pandemics in human history. (1)
In November 2002, severe acute respiratory syndrome (SARS) originated in Southern China and spread to Hong Kong (HK) in February 2003. From there, the disease rapidly spread worldwide but primarily impacted Asian countries. At the end of the epidemic in June, the global cumulative toll was 8422 cases and 916 deaths (case fatality rate of 11%). (2)
At present, COVID-19 is prevalent worldwide. In mid-November 2020, it has afflicted over 56 million people and has caused more than 1.3 million deaths, with both numbers rising by the day. Governments around the world have scrambled to build temporary healthcare facilities to treat COVID-19 patients.
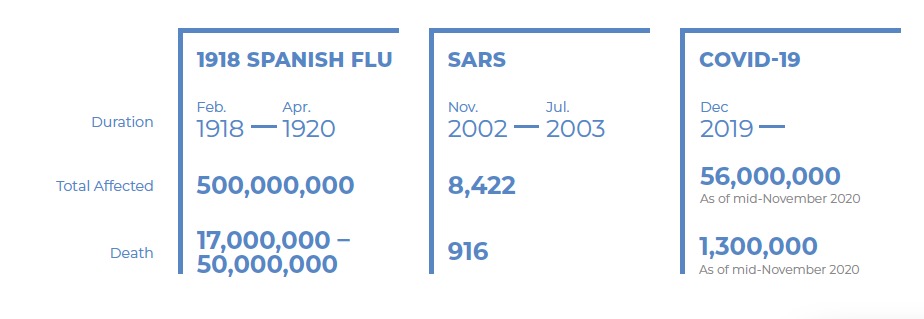
Table 1 Timeline and Statistical Comparison of Three Pandemics
To care for the overwhelming number of patients during these three viral pandemics, different styles and sophistication levels of temporary make-shift hospitals were developed across the world. These facilities varied from the historical open ward plan during the 1918 Spanish flu to the Xiaotangshan Temporary Hospital constructed in 2003 in Beijing China to combat SARS. Today, many temporary isolation healthcare facilities have been built for COVID-19 patients. They all follow the same infection control principles of contact precaution and isolation.
When planning healthcare facilities to meet future unprecedented surges in demand, we must reflect on the current chaotic situation that has occurred worldwide. We can no longer afford to take small steps learned from painful lessons each time. Viruses and diseases know no national boundaries – it is time to make revolutionary advances to be better prepared for the next pandemic.
2. The 2003 SARS Experience at Princess Margaret Hospital, Hong Kong (HK)
In late 2002, a mysterious pneumonia was beginning to impact Southern China. Rumors were spreading, but after decades of relatively good public health status, the threat of a flu pandemic was not taken seriously. At that time, the author was the Hospital Chief Executive of the Princess Margaret Hospital (PMH), a 1700-bed acute tertiary hospital, and the only designated infectious disease hospital in HK.
In late February 2003, a visitor who was carrying the SARS virus came to HK from Zhongshan, China. From the nineth floor of the M Hotel where he stayed, 17 visitors became infected and rapidly spread this super virus throughout HK and around the world to Canada, China, Vietnam, and Singapore, among other locations. One of these 17 visitors was passing through HK on the way to Vietnam. This person stayed for 1 night on the 9th floor of the M Hotel. When he arrived in Vietnam, he became ill and was admitted to a French hospital in Hanoi where he infected 63 local medical staff, including Dr. Carlos Ubani of the World Health Organization (WHO) who later died from the disease.
Another young visitor to the 9th floor of the M Hotel developed pneumonia and was admitted to ward 8A of the Prince of Wales Hospital. In this ward, he infected more than 200 medical staff and patients, resulting in a local community outbreak. One infected patient in this cohort was discharged home to Amoy Gardens where he further spread the virus throughout his block. This transmission event was related to a blocked faulty sewage system, leading to the SARS outbreak in Amoy Gardens and East Kowloon and throughout HK.
On March 27, in light of the rapid SARS outbreak in Amoy Gardens, the HK government requested PMH to be turned into a designated SARS hospital to receive newly confirmed SARS patients. The preparatory work of converting an acute general hospital into an infectious disease hospital within two days was a monumental task. It was a race against time to transfer out the existing non-SARS patients and improve infection control measures. Routine services were also withheld. At the time, PMH had only four properly built negative pressure isolation wards, with a total of eighty beds. The electrical and mechanical team rapidly installed window exhaust fans to all wards to ensure stronger air outflow, creating a relatively negative pressure environment. This is a very important measure to protect staff who work in a highly infectious environment. Subsequent air flow studies revealed that “low-level exhaust,” a system designed to direct patients’ exhaled breath downwards, kept contaminated air away from staff attending at the bedside.
Wards and beds were reshuffled and reassigned to create 720 adult and 118 pediatric SARS beds. All beds were spaced at least 3 feet apart. Notably, infection control guidelines were quite rudimentary in those days. Even the WHO was changing protocols and recommendations daily. The debate over whether SARS was transmitted by droplets and/or aerosols created much confusion in an already stressful situation. The open-plan intensive care unit (ICU) was expanded from one ward to four wards, but unfortunately, it did not have sufficient negative pressure. The preparation work was extremely difficult, both logistically and emotionally, with the need to handle staff opinions sensitively. Dr. Heymann from the WHO described this task as “Building a boat…and sailing it at the same time.”
On March 29, just two days after the official announcement, the formal role of PMH as a SARS hospital began. The hospital was immediately overwhelmed with critically ill SARS patients from the Amoy Gardens cohort. We accepted nearly 600 SARS patients in the first few days, including over 40 requiring intensive care. The ICU is a highly complex setting requiring a team of skilled and experienced staff. The rapid expansion of the ICU with staff arriving from elsewhere can be described as an orchestra lacking coordination. To further magnify the problem, these were highly infectious patients, many of whom required intubation and ventilator care. The medical staff were not impervious, and many became infected. Those were the darkest and most demoralizing days. Fortunately, with outside help and with various improvement measures, the number of colleagues infected dropped sharply, and the epidemic in HK gradually stabilized. We were fortunate that none of our infected staff died.
The SARS outbreak swept across HK rapidly, leaving us no time to think. If PMH had refused to accept its new role, the critically ill SARS patients would have been admitted to various hospitals across HK, paralyzing the entire healthcare system. This would have resulted in an uncontrolled outbreak and more infected healthcare workers. This painful decision was correctly made without regret in the overall interest of HK. After all, the containment of infection is the most crucial tool in fighting a highly contagious disease.
From February to June, PMH admitted over 1000 suspected or confirmed SARS patients, totaling one-third of all confirmed cases in HK, and nearly 60% of the Amoy Gardens SARS patients. The SARS mortality rate of PMH was among the lowest. The staff infection rate was lower than average, and all infected colleagues recovered. In this difficult situation, we made our best effort.
During the onslaught of an overwhelming pandemic, decisions are often difficult to make, usually with limited information and short deadlines. Healthcare providers are on the front lines of fighting the epidemic and are among the most affected by the disease.
3. Planning the Infectious Disease Center (IDC) at Princess Margaret Hospital
Post-SARS, two official public reviews(3)(4) were conducted with recommendations for improvements to strengthen infection control measures and improve future pandemic preparedness. One recommendation was to build the first infectious disease center in HK at PMH. This state-of-the-art high-tech design infectious disease building was put into service in the first quarter of 2007.

Figure 1 Infectious Disease Center at Princess Margaret Hospital
The seventeen-story building has a total construction floor area of 21,600 square meters. It was constructed with the most advanced technology and is designed to be versatile and functional. It can operate seamlessly with facilities in the main hospital. The IDC was completed in October 2006 and started operation in April 2007. (5)
The center provides eight independent isolation wards with 108 negative pressure isolation beds of which fourteen are intensive care beds. Each ward is composed of independent isolation rooms with either one or two beds. Each room is equipped with electric interlocking double doors, negative pressure air conditioning, and a high-efficiency particulate air (HEPA) filtration system. Special provisions include diagnostic radiology capabilities, a biosafety level-3 laboratory, and operating and delivery rooms. The building is connected to the main hospital via a link bridge for the easy deployment of resources and access to medical facilities.
The infection control team was consulted at each stage of the project to ensure that the design and physical layout of the facility met the required infection control measures. It is crucial to incorporate infection control measures in the early stages of planning and design and continue to assess them throughout the construction process. The facility design should provide separate clean and contaminated work areas and establish a one-way workflow to prevent cross-contamination.
3.1 Design Concept
The design of the infectious disease center followed four principles: 1) segregate “clean” and “contaminated” zones; 2) contain contamination; 3) control and remove contaminants; and 4) minimize physical contacts.
(1) Segregate clean and contaminated zones
The effective implementation of infection control measures follows the workflow principle of “from clean to contaminated.” Clean refers to an area that has no source of infection, and contaminated refers to an area that is likely to become a source of infection. If this principle cannot be followed, then decontamination (such as hand washing) is required. Effective infection control measures involve proper design and proper regulations throughout the ward. Patient rooms, toilets, treatment rooms, entrances, and doctor and nurse rooms with different risks must be located so that the above principles can be maintained. Additionally, equipment should be placed in the correct locations. The movement of medical staff, patients, and supplies is the main source of pathogen transmission. It is important to verify whether there is a reverse flow from contaminated zones to clean zones.
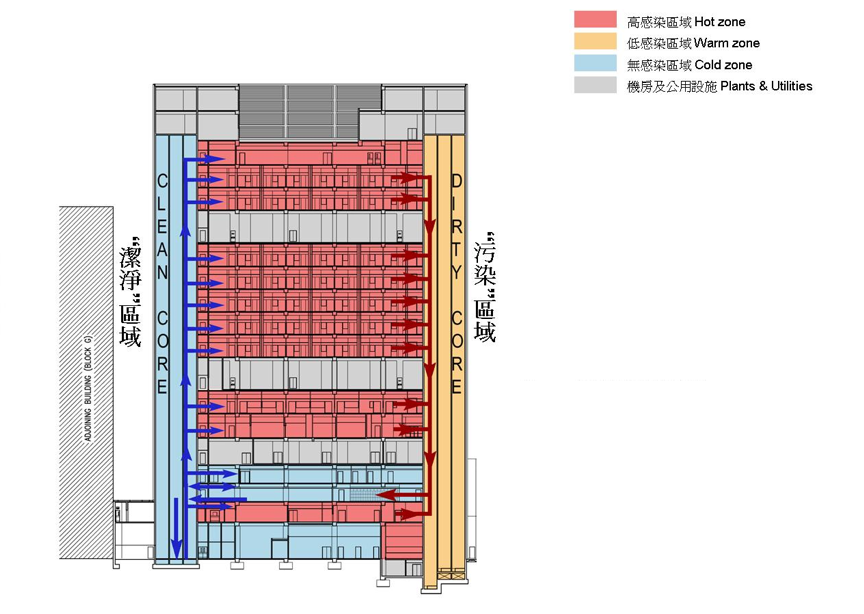
Figure 2 Separate clean and contaminated cores
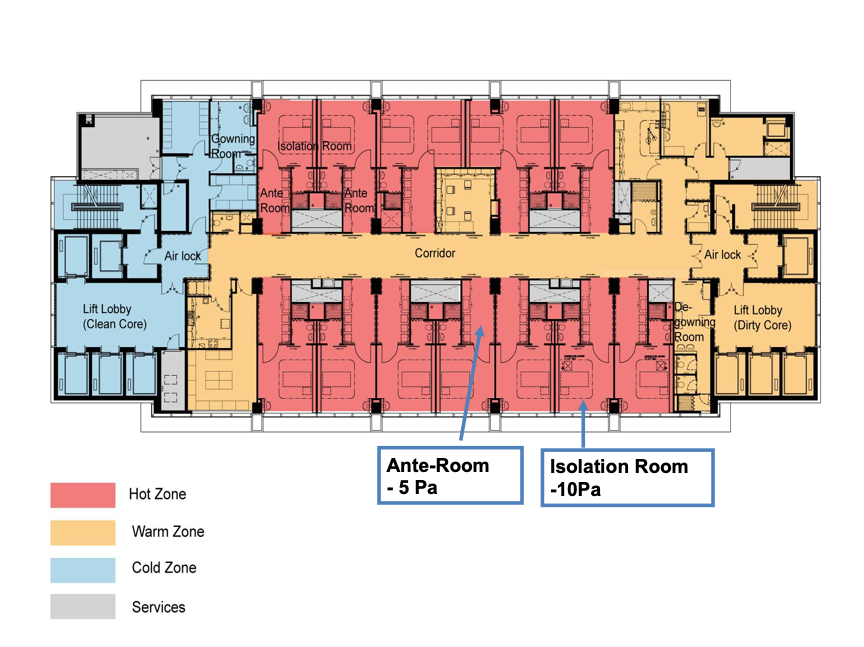
Figure 3 Separate clean and contaminated zones
The staff changing rooms are divided into a “dry–clean” area and a “wet-contaminated” area. The two sides are separated by a single row of lockers that can be accessed from both sides. Staff arrive at work through the clean entrance. They enter the clean side of the changing room, change into work clothes, and store their outerwear in a locker. After changing, they proceed to work from the clean entrance to the ward area. After finishing their shift, they enter the wet side of the changing room from the contaminated side of the ward. In the wet changing area, they shower and change into their outer clothes by retrieving their clothes from this side of the locker. They then exit from the clean side of the building.
The staff common room used for dining and rest is separated from the work area and patient treatment area. The staff lounge is a specially designed relaxation area where employees eat and rest during work. There is sufficient refrigerator space and microwaves for easily heating food. In this design, the employees do not need to leave the building during their work shift.
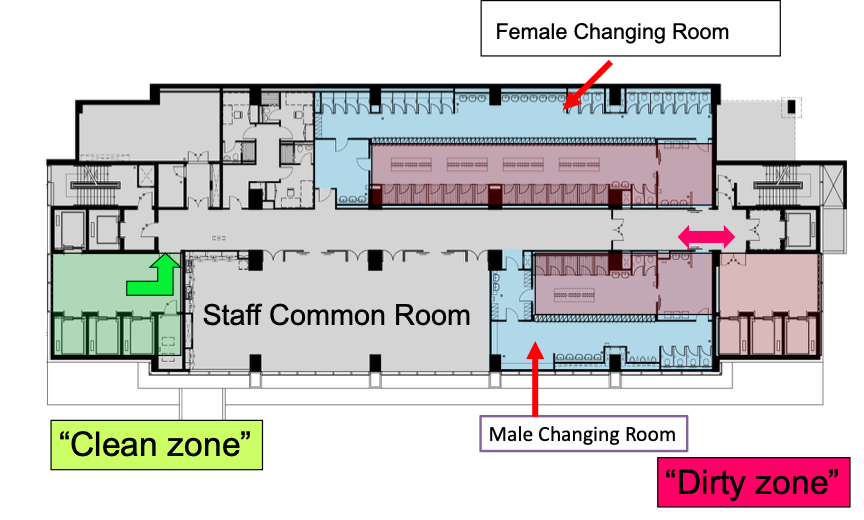
Figure 4 Layout of the staff facilities
(2) Contain contamination
To contain contamination, the air conditioning and ventilation systems are designed to allow air to flow from the clean area to the contaminated area. The pressure difference is set at −10 Pa in the patient rooms, −5 Pa in the anterooms, and 0 Pa in the corridors, thus ensuring that air flow from the nursing corridors (cleanest area) inwards through the anterooms to the patient bed areas. Before the air is discharged, it is passed through a HEPA filter to ensure that it is thoroughly disinfected before being discharged outside the building.
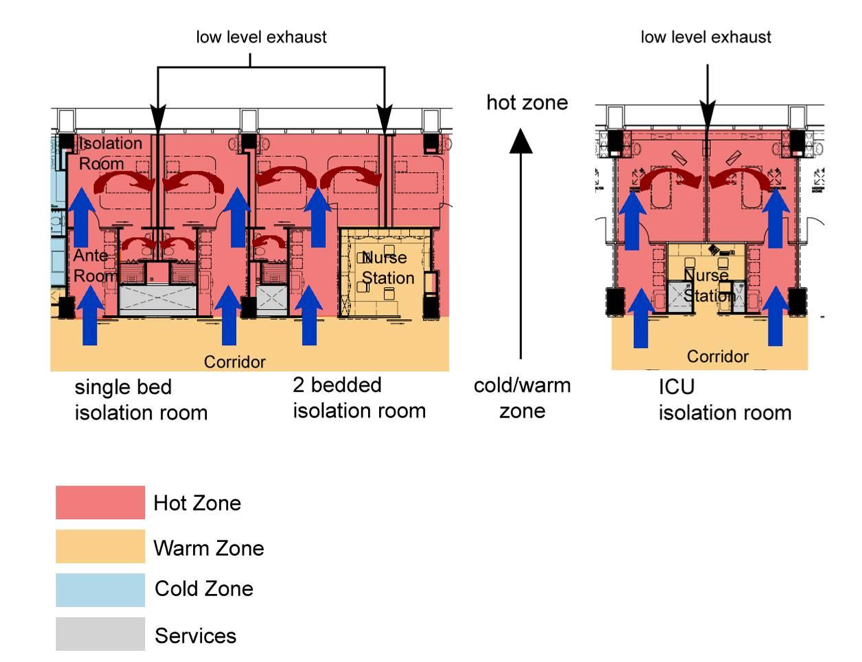
Figure 5 Design for preventing the spread of contaminants
(3) Control and remove contaminants
Adequate hand hygiene is a major factor in preventing the spread of infection. It is necessary to ensure adequate and appropriate handwashing facilities in the early design stage. In all patient areas, a combination of alcohol-based hand sanitizer dispensers and washbasins are required. The washbasin in the clinical area should ideally be equipped with a sensor faucet to prevent splashing water, and its size and height should be above elbow level to allow washing of the forearm.
Drying is an important part of the hand hygiene process. Studies have shown that all clinical areas should be equipped with tissue dispensers rather than hand dryers. The use of warm air or jet dryers in nonclinical public places may be appropriate and more cost-effective to operate, but the risk of infection increases, and they should be used with caution.
The sewage system of the center is equipped with an automatic sewage cleaning system that disinfects the sewage with high-concentration chlorine water. The patient sewage is disinfected before being discharged to the public sewer to ensure that it does not contaminate the public sewer system.
(4) Minimize physical contact
To prevent disease spread, touch-free provisions such as contact-free automatic toilet flushing systems, electronic sensor faucets, and automatic air-tight doors have been installed.
3.2 Author’s Reflection
The IDC was designed and built 16 years ago. However, many of the high-tech and advanced facilities designed at that time have remained the gold standard for isolation facilities. The recent COVID-19 pandemic is a reminder for including an adequate number of negative pressure isolation facilities when planning new hospitals.
4. Impact of COVID-19 on the Healthcare Facilities
As of the end of September 2020, the global incidence of COVID-19 continues to increase by the hour. We are facing the 2nd, 3rd, and 4th waves of the disease, with no sign of the pandemic subsiding. The fight against the COVID-19 pandemic is ongoing, and we have not yet entered the post-pandemic era.
Wuhan was the first city to report the outbreak of COVID-19. In the early days, there were shortages of emergency supplies and hospital beds because of the overwhelming number of sick patients. The local healthcare system collapsed and staff was overworked. This frightening scenario was very similar to the days when I managed SARS in 2003. Nations were taken by surprise by how fiercely COVID-19 hit every corner of the world. With prompt support from the central government, Wuhan swiftly responded by adopting three methods of managing the situation—designating hospitals, building new temporary hospitals (such as Huoshengshen Temporary Hospital), and constructing Fangcang shelter hospitals. The conversion of large-scale public venues (such as stadiums and exhibition centers) into Fangcang shelter hospitals to isolate, treat, and monitor large numbers of COVID-19 patients with mild symptoms was highly effective for controlling virus transmission and reducing mortality. These three approaches were adopted by many countries and cities. Some were successful, and some failed badly, wasting precious resources. Because the COVID-19 pandemic is ongoing, we cannot yet conclude which is the best approach in such an overwhelming situation. However, one thing that is quite certain is that despite years of disaster preparedness planning by governments, many countries have been brought to their knees by this pandemic. The traditional approaches to disaster preparedness have demonstrated intrinsic problems, such as poor economic performance, inefficiency, and a lack of flexibility. Currently, any measures that control disease transmission are considered effective and important for rapidly improving the function of a city’s healthcare system, and hence the economy. The valuable experience in Wuhan will help other countries in their battle against the COVID-19 pandemic and will also contribute to future disaster preparedness and mitigation efforts.
4.1 Public Health Perspective of Effective Pandemic Control
The effective control of a pandemic relies on a four-pronged strategy centering on:
- Early detection
- Swift contact tracing
- Prompt isolation and quarantine
- Effective containment
In the early days of a pandemic, it is most important to identify the index patient/s and conduct swift contact tracing. If this window of opportunity to trace and isolate all contacts is missed, there will be exponential spread in the community, culminating in uncontrollable community outbreak.
Quarantine is a containment strategy for people who have no symptoms but have been in close contact with a confirmed COVID-19 patient. Close contact is currently defined as being within 6 feet of a confirmed case for 15 minutes or more. Quarantine means remaining at home and limiting interactions with others for 14 days or until symptoms develop.
Isolation is a containment strategy used for people who test positive for COVID-19 or who have symptoms such as fever, cough, or shortness of breath and who need to stay away from others to prevent infecting them.
4.2 Building Temporary Quarantine Centers in HK
During the 2020 Chinese New Year, there were escalating numbers of COVID-19 cases in China, in particular in Wuhan, which overwhelmed the hospital system. At that time, we in HK contemplated the need to provide quarantine camps for close contacts of COVID-19 patients to prevent community spread. From my personal SARS experience, I realized that we must not let the virus spread because once a community outbreak occurs, the outcome is disastrous.
Our company realized the urgency of the looming crisis in HK and initiated design and planning work despite having limited information. Work started on January 28th (the 4th day of the Lunar New Year). We had to race against time to ready the quarantine camps to contain the pandemic and save lives. With strong support from the government, we launched the project at the Lei Yue Mun (LYM) Holiday Camp site. The LYM Quarantine Center project was set to provide 352 isolation units in two phases. It was built by assembling modular integrated construction (MiC) units, which were assembled at a factory in Zhuhai, transported to HK, and installed on-site. This shortened the construction period and enhanced the quality of construction and site safety. However, a detailed design plan for the MiC units was required to ensure a high-quality outcome. This was the first MiC project in HK. On completion, the project was hailed by the media as the “Hong Kong version of the Huoshenshan Temporary Hospital.”
The project design had to meet the infection control requirements of the HK Department of Health regarding spatial layout, ventilation, cleanliness zoning, indoor hygiene, infection control, and medical staff operation and workflow. Each MiC unit weighs more than 10 tons and can withstand strong winds up to a level 10 typhoon. After delivery of the MiC units on-site, only the water and electricity lines need to be connected on the spot, which greatly reduces the construction time. The structure, waterproofing, fire protection, and functions of the MiC buildings complied with the HK Buildings Ordinance and were designed in accordance with the requirements of permanent buildings. Their design and construction, including the use of materials, have been put under strict supervision and acceptance procedures.
One major hurdle of the project was difficulties in sourcing the construction materials owing to factory closures during the fourteen-day Chinese New Year holiday break. Much liaison work was required to overcome the material supply shortage, work out the MiC unit delivery logistics, and address many other concerns. Luckily, with strong support from many government departments, the problems were solved as they arose. Work at the site was carried out around the clock. The “Hong Kong spirit, Hong Kong speed” had made an impossible mission become possible. On February 28, we completed Phase I of the project and handed over site A containing 118 units, which took 600 hours to complete the design, construction, approval, and furnishing. On April 9, we delivered site B containing 234 units. In total, the project was completed in 1,320 hours.
On March 2, the first cohort of COVID-19 contacts was admitted for quarantine. From July 26, the LYM Quarantine Center further expanded its mission to provide step-down care for recovering COVID-19 patients, thus releasing valuable hospital beds for treating newly diagnosed COVID-19 patients. This is the best proof of recognition of the quality of our work.

Figure 6 LYM Quarantine Center Site A and Site B

Figure 7 LYM Quarantine Center Site A

Figure 8 LYM Quarantine Center Site B
4.2.1 Medical Input for the Project
When work first started on January 31, the LYM Camp site was already functioning as a quarantine center for quarantining COVID-19 contacts. We were aware of the psychological concerns of the construction site staff regarding working in an infected area where healthcare workers in full PPE were also working and where potential COVID-19 patients were walking outside the site boundary. Being the medical expert on the team, I took extra precautionary measures to address this. A full workforce was key for the success of this special project under especially trying times. If we did not allay their fears, the construction site staff may have refused to work there, and we may have never delivered the project on time.
Some of the measures included:
- Health talks with the site managers and site staff regarding infection control measures and general knowledge about COVID-19.
- Designing the workflow within the site area to ensure all staff entering the site underwent a temperature check and filled out a health declaration status.
- Ensuring tight control of the site boundary; site staff were provided with point-to-point commuting arrangements and five free meals per day (breakfast, lunch, dinner, afternoon tea, and supper).
- Ensuring adequate infection control measures such as handwashing facilities and providing masks, gloves, goggles, and disinfectant. The site safety officer conducted infection control patrol rounds to ensure that staff wore masks and maintained social distancing, especially during meal breaks.
- Special training on donning and doffing PPE, especially for staff handling high-risk jobs that involved contact with sewage discharge from other occupied camp sites.
4.3 Author’s Reflection
My medical role in this project yielded positive results. This project demonstrated the advantage of involving clinicians in the early design stage. Clinicians can help architects to think through potential pandemic scenarios from the users’ perspective of infection control. The airflow, sewage discharge method, and segregation of clean and contaminated zones are particularly important. Our design plan was readily accepted by health experts because the key infection control concerns were well-addressed. Regarding future healthcare facility planning, this project has demonstrated the merits of a joint team of medical professionals and architects in producing optimal outcomes, especially for the post-pandemic era.
5. Thoughts on the Building Construction in the Post-Pandemic Era
5.1 Building Future Healthcare Facilities
COVID-19 has already inflicted unprecedented global economic damage. Everyone is eager to contain the outbreak and return to normal. With the pandemic still raging, more cities are considering different types of temporary facilities for quarantining contacts or isolating convalescing patients. These facilities help to spare precious hospital beds for sicker patients. They can also act as temporary quarters for doctors and nurses who are working hard to fight COVID-19, enabling them to quarantine themselves after work and avoid potentially transmitting the virus to their families. Despite all the various measures, these temporary facilities will likely not prevent a second or third outbreak of COVID-19. However, some combination of measures may help to keep it contained so that countries can pursue less economically damaging measures, such as PCR testing, contact tracing, and quarantines, until mass vaccination is available.
As professionals in the medical and architectural fields, we need to think outside the box for how to best contain and end the present pandemic. Looking ahead into the post-pandemic era, we must figure out how to build flexibility into the design of future healthcare facilities so that we do not lock up precious resources that will remain dormant when the epidemic is over. Nor should we clamor and panic every time a pandemic recurs. In Chicago, Rush University Medical Center built its hospital tower in 2012 in anticipation of an emergency event. The center’s lobby features columns equipped with electricity and medical gases to supply patients during a surge, making it possible to readily expand both emergency department capacity and the number of isolation rooms when needed. (6) The Rambam Hospital in Haifa, Israel can convert its underground parking garage into a 2000-bed hospital if needed. (7)
Technologies also play a role in addressing infection control measures, such as providing touch-free control for lighting, temperature, and other building functions, to help avoid spreading diseases via these high-contact surfaces. The use of building materials that are less hospitable to microbes (such as copper) may also reduce the risk of surface transmission. The use of e-glass or smart glass to eliminate window curtains is another of these initiatives. A strict no visiting policy has sadly resulted in many patients dying alone. New hospital designs should help patients stay connected to friends and family by incorporating technologies such as video chat and virtual reality headsets.
5.2 Redesigning Cities to Fight Future Pandemics
More holistic approaches to making cities and buildings healthier can impact future epidemics by helping citizens to stay healthy and be better equipped to fight serious consequences when illness strikes. Bringing fresh air into buildings is important, as is improving ventilation in dense neighborhoods. Similarly, easy access to parks encourages people to stay outdoors more. In addition, providing more handwashing basins can encourage hand hygiene.
6. Conclusion
Previous pandemics have had serious global consequences for human health and the economy. However, society is forgetful of the devastating impacts that occur each time a pandemic strikes. The idea of “back to basics” does not mean going backward. We should brainstorm how to incorporate technology into the basic needs of life. Residents of the recently locked down cities surely have many reflections on their previous life of freedom. What are the simple pleasures in life that they miss most? What are the alternative options and solutions they have discovered to get by and survive? These are soul searching questions that we should ask ourselves. In addition to the loss of lives and health, what have we gained and what have we lost from the consequences of COVID-19? Society needs to stand up again, but how? How can we be smarter and better prepared when the next pandemic or disaster hits the world? We need to nurture and reboot our systems. Engaging in building healthy cities may be one solution. But this requires a high level of governmental commitment. The COVID-19 pandemic is a solemn wake-up call for everybody to stand up and act. Green environments and fresh air are basic elements of life that have been ignored by the overpowering forces driven by political and financial interests. This pandemic has brought two professions together—architects and medical workers. Our work is closely intertwined, and we should understand each other better and influence each other’s work. Together, we can build a healthier world for the next generation.
Endnotes
- Michael Rosenwald, “History’s Deadliest Pandemics, from Ancient Rome to Modern America,” Washington Post, April 7, 2020, https://www.washingtonpost.com/graphics/2020/local/retropolis/coronavirus-deadliest-pandemics/.
- Moira Chan‐Yeung and Xu Rui‐Heng, “SARS: Epidemiology,” Respirology 8 (2003): S9–S14.
- “Report of the Hospital Authority Review Panel on the SARS Outbreak,” Hospital Authority, accessed July 29, 2020, https://www.ha.org.hk/haho/ho/conjoint/123841e.htm.
- “SARS in Hong Kong: from Experience to Action,” SARS Expert Committee, last revised July 21, 2003, https://www.sars-expertcom.gov.hk/english/reports/reports.html.
- Lily Chiu, “Planning Experience of Infectious Disease Center of Princess Margaret Hospital,” Zhuyitai, February 18, 2020, https://mp.weixin.qq.com/s/sWnu-5zqKc5MGyXCGxcXvg.
- “This Is What Rush Was Built For,” Rush University, accessed July 29, 2020, https://www.rushu.rush.edu/news/%E2%80%98-what-rush-was-built-%E2%80%99.
- Judy Siegel-Itzkovich, “Rambam Parking Lot will Serve as Hospital,” Jerusalem Post, June 3, 2012, https://www.jpost.com/health-and-science/rambam-parking-lot-will-serve-as-hospital.
Author: CHIU Lee-Lee
China State Construction International Medical Industry Development Co., Ltd.



 loading......
loading......